Hip Pain Recommendations
Hip Pain Recommendations
Objectives:
- To describe evidence-based physical therapy practice including diagnosis, prognosis, intervention, and assessment of outcome for musculoskeletal disorders commonly managed by orthopaedic physical therapists
- To classify and define common musculoskeletal conditions using the World Health Organization’s terminology related to impairments of body function and body structure, activity limitations, and participation restrictions
- To identify interventions supported by current best evidence to address impairments of body function and structure, activity limitations, and participation restrictions associated with common musculoskeletal conditions
- To identify appropriate outcome measures to assess changes resulting from physical therapy interventions in body function and structure as well as in activity and participation of the individual
- To provide a description to policy makers, using internationally accepted terminology, of the practice of orthopaedic physical therapists
- To provide information for payers and claims reviewers regarding the practice of orthopaedic physical therapy for common musculoskeletal conditions
- To create a reference publication for orthopaedic physical therapy clinicians, academic instructors, clinical instructors, students, interns, residents, and fellows regarding the best current practice of orthopaedic physical therapy
Target Population
Diagnosis/Evaluation/Risk Assessment
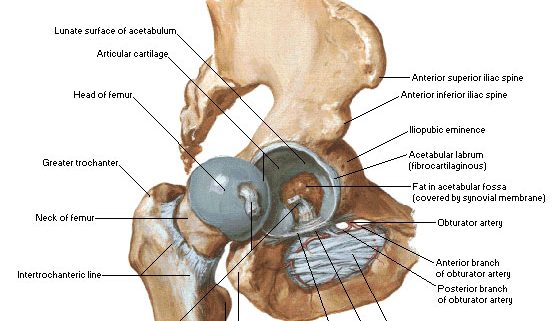
- Assessment of pathoanatomical features of the hip joint
- Assessment of risk factors (age, developmental disorders, previous hip joint injury)
- Diagnostic classification and differential diagnosis
- Use of validated functional outcome measures
- Western Ontario and McMaster Universities Osteoarthritis Index
- Lower Extremity Functional Scale
- Harris Hip Score
- Use of limitation measures
- 6-minute walk
- Self-paced walk
- Stair measure
- Timed up-and-go tests
Treatment/Management
- Patient education
- Functional, gait, and balance training through use of assistive devices such as canes, crutches, and walkers
- Manual therapy
- Flexibility, strengthening, and endurance exercises
Major Outcomes Considered
- Prevalence and risk of hip osteoarthritis
- Diagnostic accuracy (sensitivity, specificity)
- Reliability and validity of outcome measures (functional scales)
- Effectiveness of interventions in terms of pain relief, improvement of functioning, quality of life
- Adverse events associated with treatment
Major Recommendations for Hip Pain
Levels of evidence (I–V) and grades of recommendation (A–F) are defined at the end of the “Major Recommendations” field.
Impairment-/Function-based Diagnosis
Pathoanatomical Features
Clinicians should assess for impairments in the mobility of the hip joint and the strength of the surrounding muscles, especially the hip abductor muscles, when a patient presents with hip pain. (Grade of Recommendation: C)
Risk Factors
Clinicians should consider age, hip developmental disorders, and previous hip joint injury as risk factors for hip osteoarthritis. (Grade of Recommendation: A)
Diagnosis/Classification
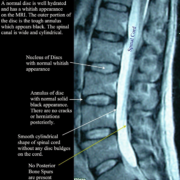
Moderate lateral or anterior hip pain during weight bearing, in adults over the age of 50 years, with morning stiffness less than 1 hour, with limited hip internal rotation and hip flexion by more than 15° when comparing the painful to the nonpainful side are useful clinical findings to classify a patient with hip pain into the International Statistical Classification of Diseases and Related Health Problems (ICD) category of unilateral coxarthrosis and the associated International Classification of Functioning, Disability, and Health (ICF) impairment-based category of hip pain (b2816 Pain in joints) and mobility deficits (b7100 Mobility of a single joint). (Grade of Recommendation: A)
Differential Diagnosis
Clinicians should consider diagnostic classifications other than osteoarthritis of the hip when the patient’s history, reported activity limitations, or impairments of body function and structure are not consistent with those presented in the diagnosis/classification section of this guideline or when the patient’s symptoms are not diminishing with interventions aimed at normalization of the patient’s impairments of body function. (Grade of Recommendation: F)
Examination
Outcome Measures
Clinicians should use validated functional outcome measures, such as the Western Ontario and McMaster Universities Osteoarthritis Index, the Lower Extremity Functional Scale, and the Harris Hip Score, before and after interventions intended to alleviate the impairments of body function and structure, activity limitations, and participation restrictions associated with hip osteoarthritis. (Grade of Recommendation: A)
Activity Limitation and Participation Restriction Measures
Clinicians should utilize easily reproducible physical performance measures, such as the 6-minute walk, self-paced walk, stair measure, and timed up-and-go tests to assess activity limitation and participation restrictions associated with their patient’s hip pain and to assess the changes in the patient’s level of function over the episode of care. (Grade of Recommendation: A)
Interventions
Patient Education
Clinicians should consider the use of patient education to teach activity modification, exercise, weight reduction when overweight, and methods of unloading the arthritic joints. (Grade of Recommendation: B)
Functional, Gait, and Balance Training
Functional, gait, and balance training, including the use of assistive devices such as canes, crutches, and walkers, can be used in patients with hip osteoarthritis to improve function associated with weight-bearing activities. (Grade of Recommendation: C)
Manual Therapy
Clinicians should consider the use of manual therapy procedures to provide short-term pain relief and improve hip mobility and function in patients with mild hip osteoarthritis. (Grade of Recommendation: B)
Flexibility, Strengthening, and Endurance Exercises
Clinicians should consider the use of flexibility, strengthening, and endurance exercises in patients with hip osteoarthritis. (Grade of Recommendation: B)
Impairment-/Function-based Diagnosis
Pathoanatomical Features
Clinicians should assess for impairments in the mobility of the hip joint and the strength of the surrounding muscles, especially the hip abductor muscles, when a patient presents with hip pain. (Grade of Recommendation: C)
Risk Factors
Clinicians should consider age, hip developmental disorders, and previous hip joint injury as risk factors for hip osteoarthritis. (Grade of Recommendation: A)
Diagnosis/Classification
Moderate lateral or anterior hip pain during weight bearing, in adults over the age of 50 years, with morning stiffness less than 1 hour, with limited hip internal rotation and hip flexion by more than 15° when comparing the painful to the nonpainful side are useful clinical findings to classify a patient with hip pain into the International Statistical Classification of Diseases and Related Health Problems (ICD) category of unilateral coxarthrosis and the associated International Classification of Functioning, Disability, and Health (ICF) impairment-based category of hip pain (b2816 Pain in joints) and mobility deficits (b7100 Mobility of a single joint). (Grade of Recommendation: A)
Differential Diagnosis
Clinicians should consider diagnostic classifications other than osteoarthritis of the hip when the patient’s history, reported activity limitations, or impairments of body function and structure are not consistent with those presented in the diagnosis/classification section of this guideline or when the patient’s symptoms are not diminishing with interventions aimed at normalization of the patient’s impairments of body function. (Grade of Recommendation: F)
Examination
Outcome Measures
Clinicians should use validated functional outcome measures, such as the Western Ontario and McMaster Universities Osteoarthritis Index, the Lower Extremity Functional Scale, and the Harris Hip Score, before and after interventions intended to alleviate the impairments of body function and structure, activity limitations, and participation restrictions associated with hip osteoarthritis. (Grade of Recommendation: A)
Activity Limitation and Participation Restriction Measures
Clinicians should utilize easily reproducible physical performance measures, such as the 6-minute walk, self-paced walk, stair measure, and timed up-and-go tests to assess activity limitation and participation restrictions associated with their patient’s hip pain and to assess the changes in the patient’s level of function over the episode of care. (Grade of Recommendation: A)
Interventions
Patient Education
Clinicians should consider the use of patient education to teach activity modification, exercise, weight reduction when overweight, and methods of unloading the arthritic joints. (Grade of Recommendation: B)
Functional, Gait, and Balance Training
Functional, gait, and balance training, including the use of assistive devices such as canes, crutches, and walkers, can be used in patients with hip osteoarthritis to improve function associated with weight-bearing activities. (Grade of Recommendation: C)
Manual Therapy
Clinicians should consider the use of manual therapy procedures to provide short-term pain relief and improve hip mobility and function in patients with mild hip osteoarthritis. (Grade of Recommendation: B)
Flexibility, Strengthening, and Endurance Exercises
Clinicians should consider the use of flexibility, strengthening, and endurance exercises in patients with hip osteoarthritis. (Grade of Recommendation: B)
Bibliographic Source:
| Cibulka MT, White DM, Woehrle J, Harris-Hayes M, Enseki K, Fagerson TL, Slover J, Godges JJ. Hip pain and mobility deficits–hip osteoarthritis: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009 Apr;39(4):A1-25. [216 references] PubMed |