The 4 Steps to Successful Sports Injury Management pt 1
The 4 Steps to Successful Sports Injury Management
.
1. Securing an accurate, reliable and detailed diagnosis as soon as possible.
Making an accurate and detailed diagnosis requires time, experience and skill.
.
A rushed or inexperienced assessment can result in a inaccurate diagnosis and an inaccurate and ineffective treatment plan.
In addition, a wrong diagnosis can result in setting unrealistic expectations and timelines.
Before proceeding to any form of treatment, your physician or physiotherapist should be able to answer the following six questions for you. Ideally you should get the answers in writing.
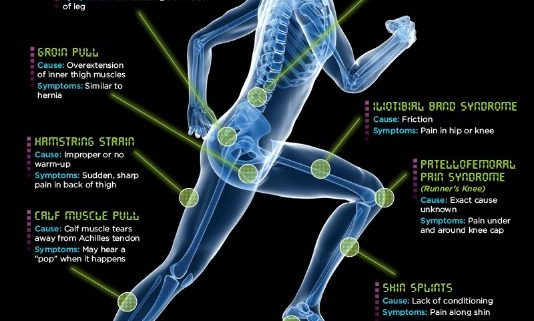
- What specific tissue(s) have been injured? (anatomical name)
- What is the least vascular tissue that has been injured (tendon? cartilage?)
- How severe is the tissue damage? (grade 1? grade 2? grade 3?)
- What is the prognosis for a full recovery of an injury of your severity? (will it heal? will it be 100%?)
- How long does it take for an injured tissue of your severity to biologically heal or mature?
- What are realistic biological timelines to see a (1) reduction of pain (2) improvement in function?
2. Creating the optimal environment to facilitate tissue repair (healing) for an adequate period of time.
The Importance of a Well Designed Treatment Plan
There are two phases in the management of musculoskeletal injuries: (1) restoration of anatomy (also known as healing) and (2) the restoration of physiology (also known as function).
As a rule, all musculoskeletal injuries require a period of protection in the early stages to allow the body to create primitive repair tissue (healing). In order to allow primitive repair tissue to mature, protection is often achieved through restricted motion at the site of injury using devices like slings, braces, casts, tape and so on.
The period of protection or restricted motion at an injury depends on a variety of factors including (1) the vascularity (blood flow) to the injured tissue and (2) the severity or depth of the tissue damage. This is information that your clinician must know about your injury in order to establish an appropriate treatment program with realistic timelines.
With each passing day, repair tissue gains tensile strength (healing) like glue setting. As soon as the repair tissue has regained enough tensile strength to withstand re-loading it, it’s critical to begin moving it again to restore physiology (functional motion and stability).
The science of restoring function through exercise or activity depends on the tensile strength of the repair tissue at each stage of healing;
- If you put too much load, too early through the repair tissue, it can cause re-injury and prolong the healing process.
- If you protect an injury too long without moving, this can cause severe stiffness, weakness and prolong the rehab process.
What we know about tissue healing;
- The absence of pain does not mean an injury has fully healed. In some injuries, repair tissue matures as slow as 1% to 2% a week. During this time, as repair tissue matures and remodels, you are vulnerable re-injury with a premature return to work, sports or other activities.
- Continuing to do activities at work or in sports, known to trigger pain, will delay tissue maturation and potentially result in permanent chronic pain.
- The presence of night pain is not a good thing and is something that needs to be assessed by a healthcare professional as soon as possible.
- The younger you are, the more likely you’ll heal faster.
- The more blood flow an injured tissue has, the more likely you’ll biologically heal faster (muscles heal faster than tendons or ligaments). With the exception of bone, the whiter in appearance of a injured tissue in an anatomy book, the slower you can expect it to heal.
- Genetics do play a role in tissue healing. Some people do heal faster than others.
- If you smoke or have peripheral vascular disease (often associated with diabetes), you will likely heal at a slower rate than a non-smoker.
- The greater the depth of tissue injury, the longer it will likely take to heal.
Designing the best treatment plan depends on;.
- An accurate and reliable diagnosis
- Biological knowledge of how your injury heals, how well it heals and how fast it heals.
- Biological knowledge of exactly what type and dose of activity works best for a specific diagnosis at each stage of tissue healing
- Biological knowledge of what activities and exercises can actually make a condition worse and potentially cause permanent chronic pain.
3. Restoring physiological functional capacity and individual skills to return to play.
The single most important ingredient in the rehabilitation of any bone or joint injury is safe and appropriate exercise at each stage of tissue healing (early, middle, late). The earlier a patient is able to start exercise and the more rehab exercise a patient can do at home, the faster they’ll return to work or sports.
The Importance of Exercise Rehabilitation
There are two phases to managing any musculoskeletal injury; (1) the restoration of anatomy (repair tissue formation and maturation to withstand load) and (2) restoration of physiology (rehabilitation to return to full function).
In order to allow tissue healing to take place, there is always a period of protection at the site of injury.
Protection typically takes place through some form of immobilization (sling, brace, cast, etc).
The purpose of protection is to create the right environment for sufficient primitive healing to take place before removing the protection.
Unfortunately protecting an injury results in disuse atrophy (weakness & loss of mass) of surrounding muscles,loss of muscular power and endurance, joint stiffness, loss of proprioception and motor program performance (individual work or sports skills).
.
Returning to work or sports without restoring full motion, flexibility, strength, endurance and motor skills increases the risk of sub-par performance and the risk of re-injury.
Warning: Inappropriate exercises for your condition can cause re-injury and make your injury more severe (worse).
Active exercise is required to restore the effects of protection (see above).
As a rule, the earlier that exercise can be re-introduced at the site of injury, the better.
Unfortunately doing inappropriate exercises or too much exercise can actually cause more tissue damage and delay healing.
Exercise selection and dose is determined by a variety of biological factors related to the diagnosed condition, time and a patient’s profile. One type of exercise may help one patient but make another patient worse.
Personal Training is not Physical Therapy.
Your safety is always the top priority when exercising, especially with a known medical condition, if you are taking medications, after an injury or after surgery.
Regrettably, one of the most common causes of recurrent pain and injury, is performing inappropriate exercises and/or exercises at an inappropriate dose to early after injury. This often occurs when patients download rehab exercises off the internet or hire a personal trainer.
Personal trainers are not licensed healthcare professionals and there are no educational requirements to call yourself a personal trainer. Personal trainers are not governed by a licensing body, there is no medically recognized certification and trainers not required to carry professional (malpractice) insurance. In other words, anyone can call themselves a personal trainer.
Although personal trainers can be very helpful there is a difference between ‘exercises to get fit’ and ‘rehabilitative exercises’.
The science of rehabilitative exercise is;
- Knowing whether an exercise is appropriate or inappropriate for a given condition and a client’s medical profile at a given stage of tissue healing or
- Knowing whether the dose of a given exercise is appropriate or inappropriate for a given condition and a client’s medical profile at a given stage of tissue healing.
Rather than trusting exercises from a website or a friendly personal trainer, we strongly encourage you to ask your family physician or physical therapist for the name of an individual personal trainer in your community that they trust and recommend you to work with. Ask your family physician or physical therapists to write your personal trainer a note outlining your condition, your medical profile and any contra-indicated exercises they feel are too risky to perform for your condition.
4. Making the most informed return to practice and play decision
Returning to sports prematurely, without (1) the physical fitness, (2) the sports-specific skills or (3) the mental confidence to perform are the three biggest reasons why most athletes fail to return to sports successfully.
Returning prematurely can lead to;
- Increased risk of re-injury
- Increased risk of sub-par performances (struggling to achieve sports goals without the necessary fitness or individual skills)
- Increased risk of secondary injury (i.e. unable to move quickly out of the way of an opponent due to a knee injury then sustaining a new injury such as a concussion)
- Increased risk of psychological depression & withdrawal from others (struggling to meet expectations)
- Increased risk of altered communication with coaches and teammates (struggling to meet expectations)
- Increased risk of losing of interest in the sport (no longer enjoyable if their performances are poor or the pressure to achieve or lead is too great)
- Increased risk of quitting or retiring prematurely from the sport for all the items listed above.
Must Answer “Yes” to ALL of the Following Questions
- Has repair tissue at the site of injury had adequate time to restore sufficient tensile strength to withstand the unrestricted demands of the given sport?
- Has the athlete restored full painfree range of motion at the site of injury; full muscular strength, power and endurance; normal dynamic proprioception at the affected joints?
- Has the athlete seen a physician and received medical clearance to return to unrestricted practice?
- Has the athlete restored their ability to perform their individual sport-specific skills with confidence, precision at full speed, with the endurance to repeat the skills as needed WITHOUT an immediate or delayed onset of symptoms within 24 hours?
- Does the athlete feel confident in their physical and psychological abilities to return to play and excel?
- After the athlete has participated in unrestricted practices without a return of symptoms, have they seen a physician and been cleared to participate in unrestricted competition?
Default: “If in doubt, keep them out”
The best insurance for a successful return to sports is securing clearance from the most experienced healthcare professional familiar with both the demands of the individual sport, but also the culture of the individual sport.
Calgary Sports Medicine